Understanding IBD
There are two main types of inflammatory bowel disease (IBD): Crohn’s disease and ulcerative colitis (UC). Each affects the digestive tract. Both are chronic and are considered autoimmune disorders.
Actor portrayal
The “I” in IBD is inflammatory
Your immune system protects your body from germs, infections, and other unwanted intruders. With IBD, your immune system attacks what it shouldn’t—your digestive tract. And this battle creates inflammation, which can do damage and get worse over time. In some people, the damage can be serious enough that surgery is needed.
Learn about types of IBDWhat are the common symptoms of IBD?
The symptoms of IBD can be similar to symptoms of other conditions. People with IBD often experience symptoms in waves of flare-ups (when symptoms are active) and remission (period of time in between flare-ups when you experience few to no symptoms). Having some or all of these symptoms does not mean you have IBD; only your healthcare provider can tell you that.
| Symptoms | More commonly seen in Crohn’s disease | More commonly seen in ulcerative colitis |
| Diarrhea or changes in bowel movements | ||
| Stool with blood or mucus | - | |
| Bowel Urgency | - | |
| Malnutrition | - | |
| Mouth sores | - | |
| Abdominal pain (or stomach pain or cramping) | ||
| Fatigue | ||
| Nausea | ||
| Weight loss |

Causes and risk factors
The exact cause of IBD isn’t clear.
A person may develop IBD due to the interaction between the genes they inherit from their parents and environmental factors (such as where they live and their lifestyle). Together, these factors could trigger an immune response.
IBD’s impact on the body

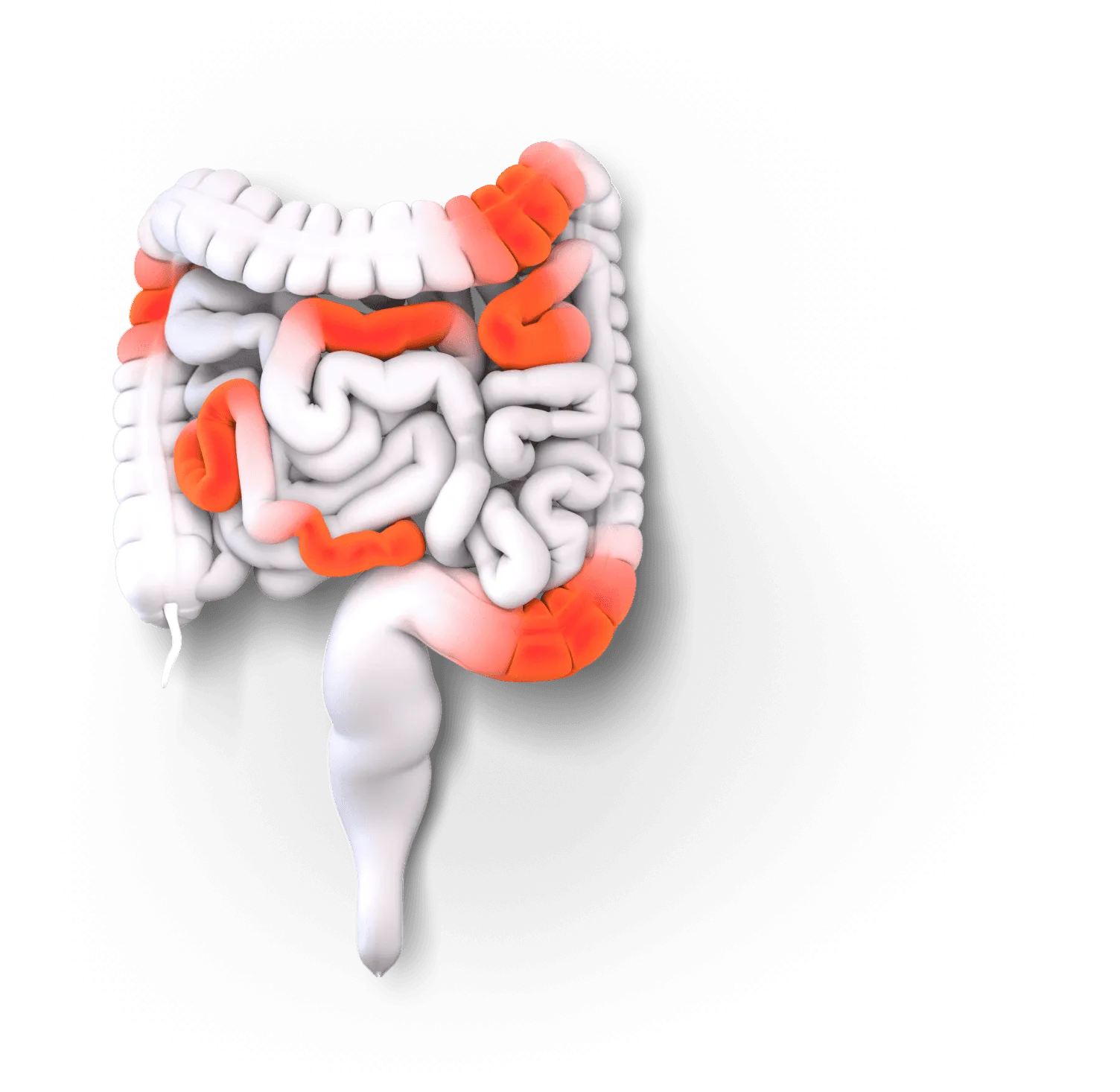
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus.
It commonly impacts the end of the small intestine and the beginning of the large intestine. Inflammation can affect all layers of the intestinal walls and cause patchy damage, affecting some areas but not others. Crohn’s is usually progressive, which means it’s likely to get worse over time for some people.
Learn More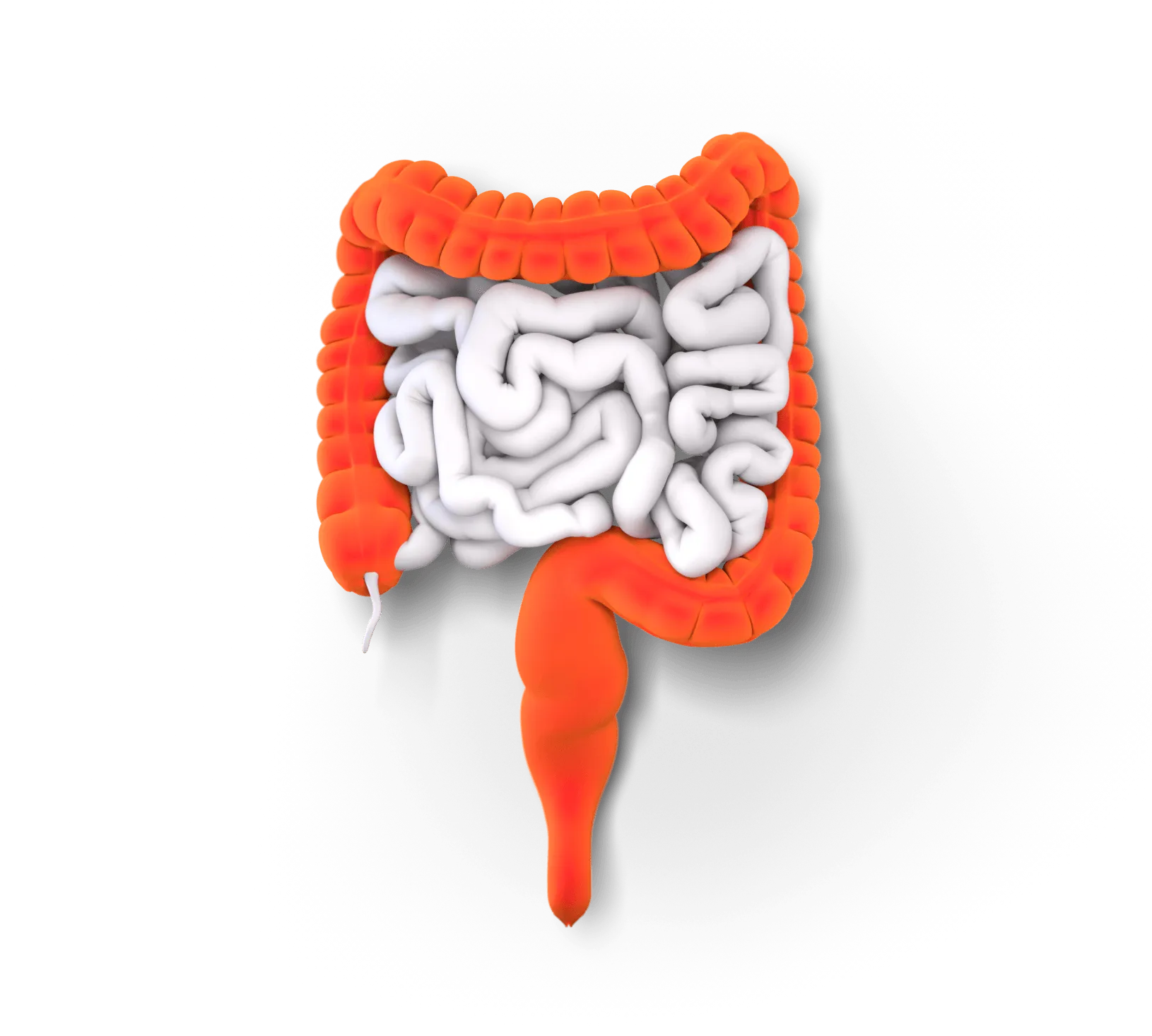
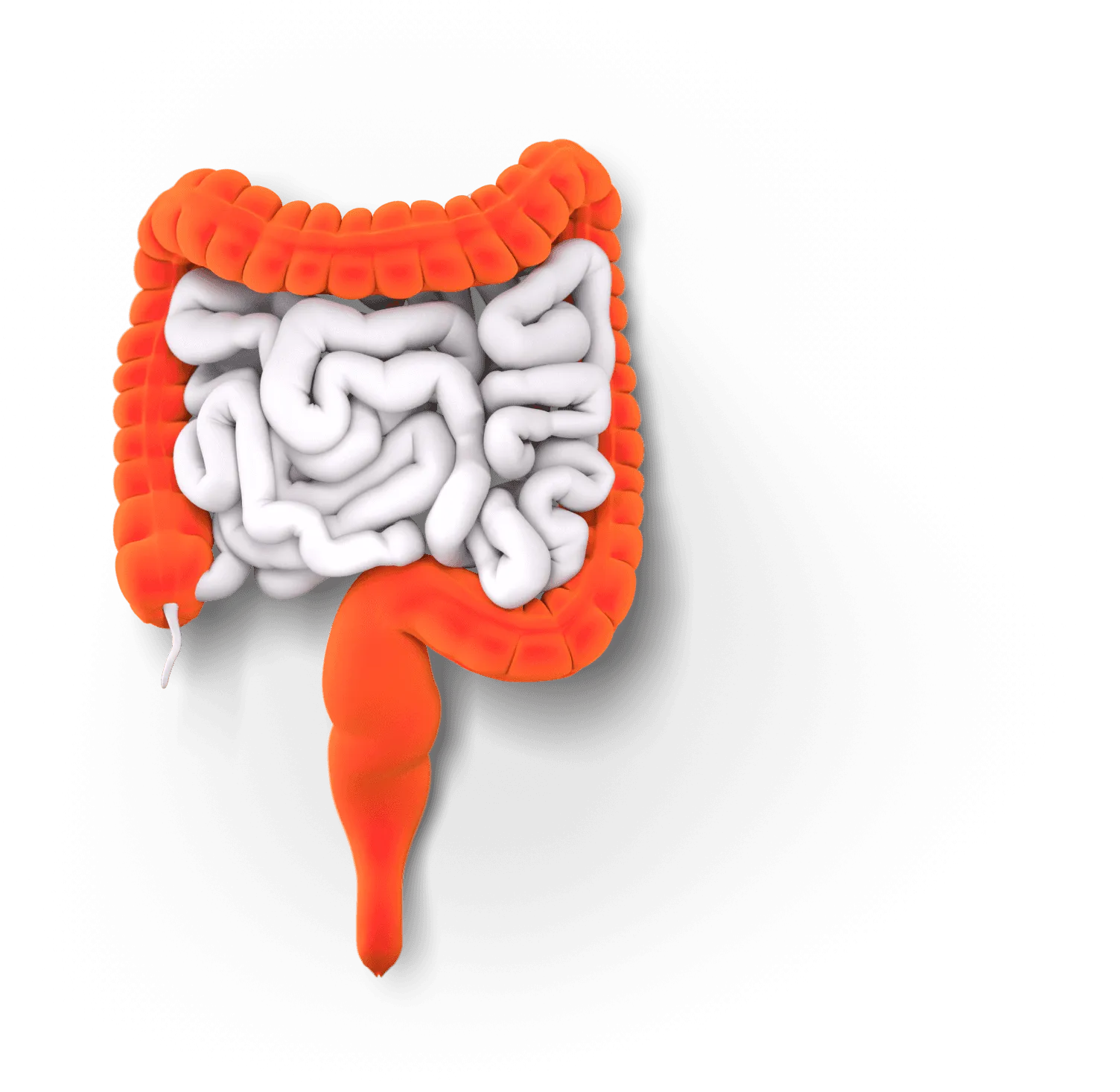
Ulcerative colitis affects the large intestine (colon and rectum).
It typically starts at the rectum and spreads up through the colon. Inflammation impacts only the innermost layer of the large intestine. It causes swelling and ulcers, or sores, all along its path, leaving no healthy tissue. UC can be progressive in some people. That means it can get worse over time.
Learn MoreConditions commonly mistaken for IBD
Irritable bowel syndrome (IBS) and celiac disease share a lot of symptoms with IBD and are often mistaken for one another—but they’re different conditions. Talk with your care team to learn more about these conditions.
| | IBD | |
| Chronic condition | ||
| Affects the digestive tract | ||
| Symptoms can include stomach pain and changes in bowel movements | ||
| Causes inflammation | - | |
| Causes symptoms beyond the digestive tract | - | |
| Autoimmune disease | - | |
| Damages the digestive tract | - | |
| Chronic condition | ||
| Autoimmune disease | ||
| Can cause long-lasting problems | ||
| Can interfere with getting proper nutrients | ||
| Triggered by | Interactions between genetics and the environment | Foods that contain gluten |
| Can cause symptoms beyond the digestive tract | - |

Shari Living with UC
My doctor told me to educate myself about IBD and let me tell you, I did.See Shari’s story
Featured
resource
Living with IBD Podcast
Listen in on real conversations people with IBD are having. They could shed some light on what you’re going through.
Featured episode
IBD and intimacy
See all episodes
Get the latest sent straight to your inbox.
Sign up